The world is in the midst of an antibiotic resistance crisis that contributes to the deaths of nearly 5 million people a year. But bacteria aren’t the only mutating organisms we have to worry about.
Fungal infections are also more adaptable than our medicine, creating a “silent epidemic” that needs to be addressed urgently, according to some researchers.
Molecular biologist Norman van Rhijn from the University of Manchester in the UK, explains: “The threat of fungal pathogens and antifungal resistance, although a growing global issue, is not for that matter.
In September this year, the United Nations held a conference in New York City on antimicrobial resistance, which includes discussions about bacteria, fungi, viruses or resistant organisms.
Ahead of this event, van Rhijn and an international team of scientists are urging governments, the research community, and the pharmaceutical industry to “look beyond just bacteria.”
Fungal infection, they write in letters for The Lancet, they are left out of many ways to deal with biological resistance.
Without care and prompt action, some serious fungal infections, which now infect 6.5 million people a year and kill 3.8 million people annually, can become even more dangerous.
van Rhijn and his colleagues, from civil society, say: “The unsustainable focus on bacteria is because most of the drug resistance problems in the past decades have been caused by invasive fungal diseases , largely unrecognized by the public and governments alike,” write van Rhijn and his colleagues, from the institutions. China, Netherlands, Austria, Australia, Spain, UK, Brazil, US, India, Türkiye and Uganda.
In 2022, the World Health Organization published the List of Fungal Pathogens – “the world’s first attempt to prioritize fungal pathogens”.
Bacteria that were considered the most dangerous to human health include Aspergillus fumigatus, which comes from mold and infects the respiratory system; candida, which can cause a yeast infection; Nakaseomyces glabratusthat can infect the urogenital tract or blood; and Trichophyton indotineaewhich can infect the skin, hair and nails.
Elderly or immunocompromised people are most at risk.
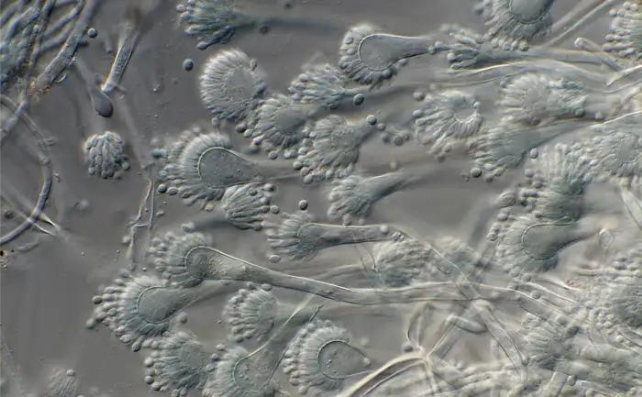
Compared to bacteria or viruses, fungi are more complex organisms, very similar to animals in their structure. This makes it difficult and expensive for scientists to develop drugs that kill fungal cells without damaging other vital cells in the body.
“To treat serious or invasive fungal infections, there are only four classes of antifungals available and resistance is now the rule rather than the exception for the current classes,” write letter writers.
In the past few decades, promising new antifungals have emerged, but the arms race between pathogen and medicine is being accelerated in part by the agrochemical industry.
“Even before [these drugs] reach the market after years of development and clinical trials, fungicides with similar mechanisms of action are produced by the agrochemical industry that cause resistance for important future pathogens first,” explain the researchers in their letter.
“Antifungal protection is necessary for food safety. The question is how do we balance food safety with the ability to treat current and future fungal pathogens?”
It is a conundrum that has been discussed for a long time for antibiotics but not so much for antifungals. Van Rhijn and his team are advocating a global agreement to limit certain antifungal drugs for specific purposes, as well as cooperative laws to balance food security and health.
The United Nations meeting in September “must serve as a starting point” for a systematic and diverse approach to anti-viruses, the researchers conclude.
No germs should be left behind.
The lesson was published in The Lancet.
#Deadly #Fungus #Infections #Silent #Epidemic #Scientists #Warn


